
Breast reconstruction is a surgical procedure designed to restore the shape and appearance of the breast following a mastectomy or lumpectomy. It can be performed at the time of cancer removal (immediate reconstruction) or at a later date (delayed reconstruction). Every woman’s journey is personal, and our goal is to help you explore the options that best align with your body, lifestyle, and vision for the future.
Expert Breast Reconstruction Surgeons in Atlanta, GA
Dr. Page and Dr. Urquia specialize in breast reconstruction and often operate alongside Dr. Mackay, forming a collaborative team approach that is synergistic and deeply patient-centered. This unique partnership allows us to deliver exceptional care, combining expertise to restore not only your breasts, but also your health and sense of self.
Our practice is highly sought after for the time and attention we devote to each patient. We take the time to truly understand your goals and tailor your surgical plan to achieve natural, beautiful results. We recognize that this may be one of the most difficult times in your life—and we’re here for every step of the journey. We invite you to share your fears, hopes, and victories with us. You are not alone.
LUMPECTOMY RECONSTRUCTION OPTIONS
A lumpectomy is a surgical procedure in which the affected portion of the breast is removed, often guided by a wire or clip placed by radiology. Depending on the location of the tumor, this may leave an undetectable defect after tumor removal. Sometimes, it may leave a very visible defect. In these cases, patients are referred to reconstruction surgeons to see if there will be options to reposition the remaining breast tissue to fill in the hollow area that the tumor removal leaves behind. This is called an oncoplastic closure.
Repositioning the breast tissue in this manner often allows for a rejuvenated or lifted appearance to the breast. It also allows for the breast oncology surgeon to remove more tissue than they would have if they did not work with a reconstructive surgeon, which lowers the rate of positive margins. This is an excellent approach if there is enough remaining breast tissue to recreate a shapely breast mound after the tumor removal. It is often difficult to tell which side the cancer was on after the reconstruction is finished, as the other breast is lifted and/or reduced to match.
It is important to remember that a lumpectomy is most often combined with radiation therapy when performed for breast cancer. There are some exceptions to this, so it is important to discuss this with your breast oncology surgeon as well.
MASTECTOMY RECONSTRUCTION OPTIONS
A mastectomy is a more dramatic approach to surgically treating breast cancer or removing breasts in a preventative manner. The breast tissue is removed from underneath the skin, leaving healthy areas of skin behind. There are many factors that go into deciding what the best reconstructive option is for you. This conversation usually takes a long time to go over, so please bring a friend or family member or a way to take notes. It is not a one size fits all, and most often not a one-and-done surgery.
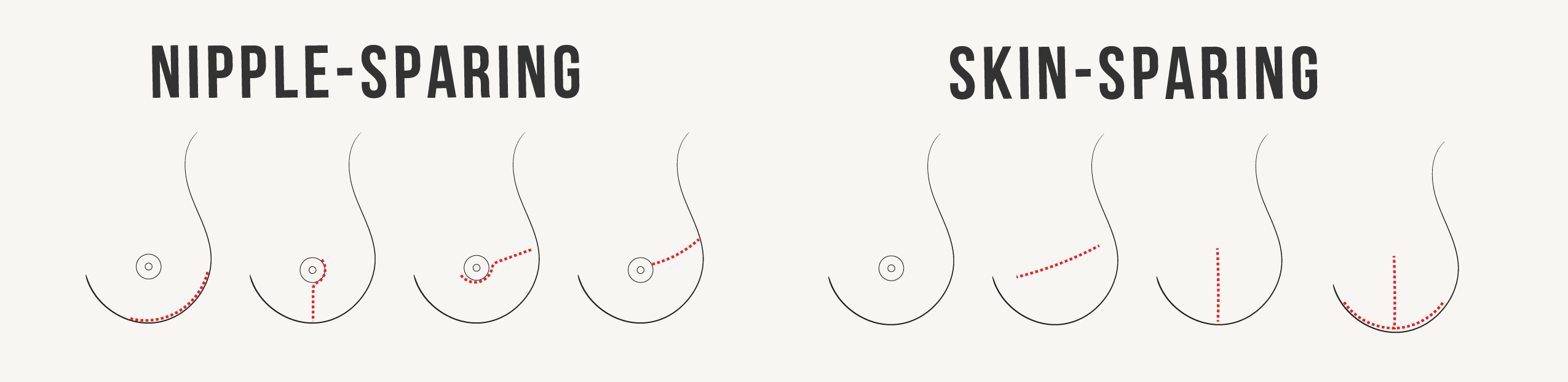
There are two primary types of mastectomy: nipple-sparing mastectomy (where the nipple is preserved) and skin-sparing mastectomy (where the nipple is removed). The nipple may need to be removed if:
- The tumor is too close to it
- It loses its blood supply during surgery
- It sits too low on a long or ptotic breast
- The patient prefers to have it removed.
Several incision patterns can be used for mastectomy, each with specific benefits and limitations based on anatomy, cancer location, and reconstructive goals. If nipple preservation is not initially safe or advisable due to large breast size, we may recommend a breast reduction first. In some cases, patients with breast cancer may be candidates for an oncoplastic lumpectomy with reduction, allowing us to reshape the breast while removing the tumor. A delayed mastectomy can then be performed about three months later, which may improve the chance of safely preserving the nipples.
Once the mastectomy is done, the reconstruction may be done at the same time if the blood flow to the skin looks good enough (it usually does). If it is not done, there are typically options to reconstruct the breast in a delayed fashion, but they may come with their own set of challenges. The below describes the main categories of breast reconstruction after mastectomy.
AESTHETIC FLAT CLOSURE
Some women find it empowering to choose a flat closure after mastectomy. It is a great option for patients who do not want to bother with long-term upkeep with an implant reconstruction, or go through a larger operation involving another body part for a flap reconstruction. It is lower risk for a patient with many medical co-morbidities. In some cases, it is very difficult to undo without leaving visible scars, so you should discuss this with your surgeon to see if this is the best option for you long term.
One things to note about flat closures is that it is not always truly flat. If the chest wall is deep compared to your belly, the flat closure may give a very hollow appearance to the chest. There may be concave and deflated looking areas depending on how much extra skin you have to start, and how much extra fatty tissue the breast surgeon removes. This may require a revision surgery (or two) to add some fat so the final contour will be smoother and truly flat.
IMPLANT BASED RECONSTRUCTION
The majority of women who undergo reconstruction will choose implant based reconstruction. Because of the lack of soft tissue coverage, we almost always use gummy-bear type silicone implants for this option. This approach is ideal for patients who prefer a shorter surgery and recovery time, but it does require some upkeep down the road (swapping out implants every 10-15 years). The final outcome of the reconstruction is highly influenced by the quality of the skin after the mastectomy is done.
Implant vs Tissue Expander
Depending on your desired final breast size and the quality of your skin after mastectomy, either a breast implant or a tissue expander may be placed during your initial surgery. Each option has its advantages, and the choice depends on your anatomy and goals.
A direct-to-implant reconstruction is ideal for women whose breast skin envelope closely matches the size and shape of the desired implant—typically in the A to C cup range. In these cases, the skin can safely support the implant right away.
Placing a larger or heavier implant immediately can strain the healing skin, which may compromise blood flow and increase the risk of complications. For this reason, larger-breasted patients may actually benefit from a tissue expander, even if they don’t need to stretch the skin. The expander gives the skin time to heal before gradually creating a safe space for a larger implant. Tissue expanders are also a good choice for smaller-breasted women who wish to increase their breast size as part of the reconstruction process. In these cases, expansion happens slowly over time to ensure the skin adjusts comfortably.
Prepectoral vs Subpectoral Position
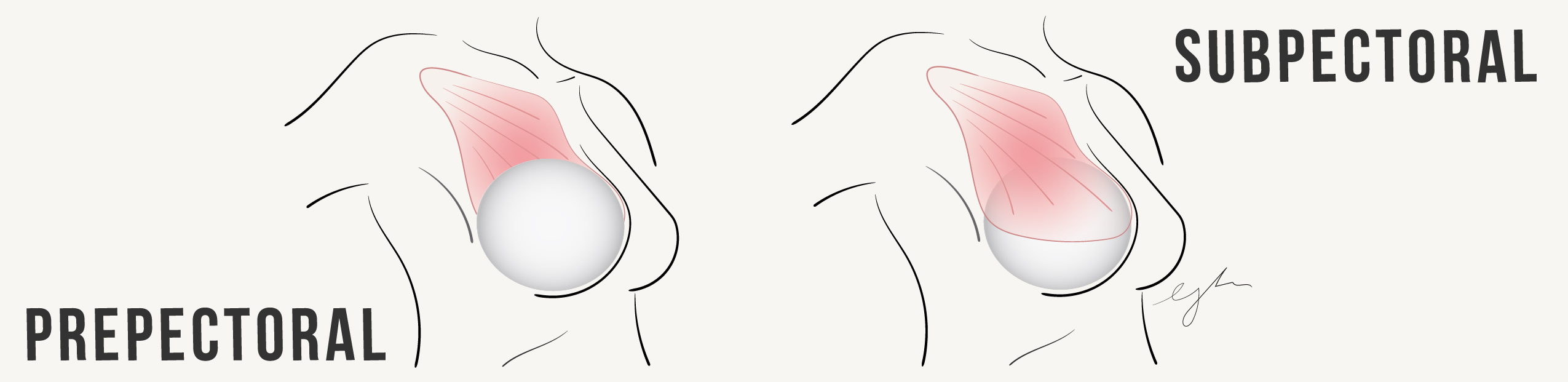
The two options for placement of the implant or expander is either above the pectoralis muscle ("prepectoral") or below the pectoralis muscle ("subpectoral"). The best option depends on your body type and skin quality, whether you've had or will need radiation, your activity level and lifestyle, and your personal preferences and goals.
Let's talk about prepectoral reconstructions. An implant above the pectoralis muscle is secured with a soft tissue support material, whether it be a biologic material like acellular dermal matrix or a synthetic mesh. This keeps the implant positioned in place. The benefits to prepectoral reconstructions are less postoperative pain, faster recovery, no animation deformity and sometimes a more natural-looking movement. For this to be successful, it requires for the remaining mastectomy skin to have enough fat under the skin so the edges and rippling of the implant do not show through the skin. It is not always the best option for very thin patients.
Subpectoral reconstructions are performed for patients who are very thin or who are left with very thin mastectomy skin flaps. It offers better protection and coverage in thin patients and may offer a smoother transition from your chest wall to the breast mound. The disadvantages are that it causes more discomfort after surgery, has a longer recovery time, may feel tight long-term, and the skin and breast may animate with muscle use. A soft tissue support material is also used with this option to best shape the breast mound.
Whichever we decide, we strive to delivery a beautiful reconstruction that will enable you to look and feel great in whatever you desire to wear, and also a reconstruction that will allow you to enjoy your favorite pasttimes without restrictions. We firmly believe in incorporating physical therapy in your recovery so we can get you back to doing all the things you love to do!
TISSUE BASED RECONSTRUCTION
Some women choose autologous or tissue based reconstruction. This is a great option for patients who (1) are young who may need multiple implant exchanges in their lifetime, (2) have failed implant reconstruction, (3) are starting with a flat closure, or (4) have a radiated breast causing tightness, pain, or significant asymmetry. It does leave long scars at the donor site, but the scars are often hidden in most garments and swimwear. Any time we move tissue from one part of the body to another, it leaves scar tissue and numbness at the donor site and has a 1-2% risk of losing blood flow to the newly created breast. We work together to find the very best option for you to minimize these risks.
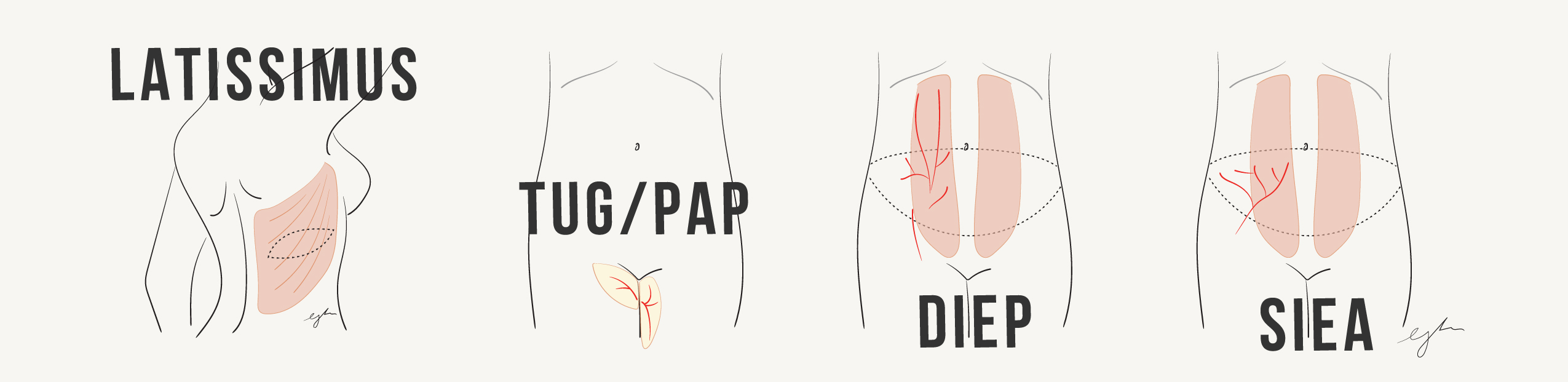
Latissimus flaps are used sparingly when patients may need more healthy skin to create a breast mound, often over an implant or expander. This is used in patients who may have had radiation in the past, or have significant areas of skin that need to be removed due to tumor involvement. IT is a good option for patients who have had prior tummy tucks or are otherwise not a good candidate for abdominal based flap reconstruction.
TUG and PAP flaps are thigh based flaps. These are good options for patients who do not have an adequate abdominal donor site. They are typically small in size, so two flaps are often stacked to create one breast. It is usually not a good option to create a larger breast.
DIEP FLAP RECONSTRUCTION
DIEP flap reconstruction is the gold standard in autologous breast reconstruction and our preferred approach. It allows us to restore the breast using a patient’s own tissue while simultaneously enhancing abdominal contour - often delivering a truly transformative result. We are proud to be one of the busiest DIEP flap practices in Atlanta, with a strong commitment to delivering natural, beautiful outcomes. In many cases, we recommend delaying the procedure to optimize shaping of the breast mound and allow patients time to reach their goal weight or a body mass index (BMI) under 30, which supports the safest and most aesthetic result.
RESENSATION
During a mastectomy, the sensory nerves that travel through the breast tissue are disrupted, often leaving the remaining breast skin feeling numb. This loss of sensation can deepen the emotional impact of surgery and carries functional consequences as well—such as the risk of unintentional injuries or burns, since patients may not feel heat or pain in the affected area.
Over the past two years, we have routinely incorporated nerve grafting techniques into our reconstructions. By identifying injured nerve endings and connecting them to nerve grafts, we aim to guide nerve regrowth toward the nipple or central breast skin. While the success rate is currently around 60–70%, we have seen meaningful return of sensation in many patients.
Although insurance coverage for this procedure is still limited, we are encouraged by growing recognition and increasing approval rates among insurers.
SECONDARY REVISIONS
Many women choose to undergo a reconstruction revision after their initial surgery. At the time of mastectomy, we often have limited control over the final shape, size, and contour due to factors like skin thickness and blood flow. A revision surgery allows us to refine the results, enhancing breast shape, volume, and symmetry. These procedures are typically covered by insurance, performed on an outpatient basis, and do not usually require drains. Recovery is generally much faster and more comfortable than the initial surgery.
COMPLICATIONS
Mastectomies carry a relatively high complication rate due to the large surface area involved and the reduced blood supply to the tissues, which can pose challenges for healing and reconstruction. The below are common complications seen after mastectomy:
Wound Healing Issues -Delayed healing or wound breakdown
Skin or nipple necrosis (especially in nipple-sparing mastectomies)
Infection - Can range from mild redness to serious deep infections May require antibiotics or surgical washout
Bleeding or Hematoma - Accumulation of blood under the skin. May require drainage
Seroma - Fluid buildup under the skin May require aspiration or drain placement
Loss of Sensation - Most patients experience numbness in the chest due to severed nerves
Pain or Neuropathic Pain - Sharp, burning, or chronic pain in the chest wall or axilla
Shoulder or Arm Stiffness - Especially if lymph nodes are removed Lymphedema Swelling of the arm due to lymph node removal or radiation
Complications after implant based reconstruction
Capsular Contracture - Scar tissue tightens around the implant causing firmness or distortion
Implant Malposition or Rippling - Visible or palpable folds, asymmetry, or migration. May require revision or fat grafting
Implant Infection or Exposure - May require implant removal
Animation deformity - May require pocket change to above the muscle
Need for Revision Surgery - Common over time to address changes in shape, symmetry, or complications
Fat necrosis or oil cysts - After fat transfer. May require imaging, biopsy, steroid injection or surgical removal
Complications after tissue based reconstruction
Flap Loss (Partial or Total) - If blood flow is compromised. May need to be repaired immediately, removed or replaced at a later date.
Fat Necrosis - Lumps of firm tissue due to poor fat perfusion
Abdominal Wall Weakness or Hernia - Related to tissue harvestin. We try to reduce abdominal wall weakness by minimizing muscle dissection and nerve transection at the time of harvesting the DIEP flap.
Longer Recovery Time - Due to dual surgical sites (chest and abdomen)
Microvascular Complications - Rare but serious—can include clotting of blood vessels in the flap. May need to be repaired immediately, removed or replaced at a later date.

Copyright 2025 Silk Plastic Surgery. All Rights Reserved.